Weight Loss for Women: Hormones, Health, and Results
Women often tell me they feel like their bodies are working against them. A plan that helped a friend drops only a pound or two, then stalls. A heavy week of travel and sleep loss adds five pounds that will not budge. The pattern is real. Female physiology, from menstrual cycling to pregnancy to perimenopause, changes appetite, water balance, insulin sensitivity, and the way we deposit fat. A smart approach acknowledges that landscape rather than fighting it.
I have guided hundreds of women through safe weight loss across different life stages, from first jobs to life after hysterectomy. The most consistent wins come from combining science based weight loss strategies with lived reality: work schedules, child care, cultural food traditions, and the nonnegotiables that keep a life whole. What follows is a practical map to understand hormones, choose an evidence based path, and decide when a physician guided weight loss plan makes sense.
Why women’s bodies gain and lose weight differently
Estrogen and progesterone sit upstream of insulin, leptin, and ghrelin. They influence how hungry you feel, how full you get, and where your body stores energy. During the follicular phase, roughly days 1 to 14 of a typical cycle, estrogen rises and insulin sensitivity is usually better. Many women feel more energetic and find cravings easier to manage. During the luteal phase, progesterone climbs and resting energy expenditure can increase by 50 to 150 calories per day, yet hunger often rises more than that. Bloating from fluid shifts can mask fat loss on the scale by 1 to 4 pounds. Without understanding this, many people conclude a plan has failed when it is only normal physiology.
Pregnancy and postpartum add layers. Weight gain targets are appropriate, and insulin resistance increases naturally. After delivery, sleep fragmentation and prolactin shifts drive stronger appetite signals. Breastfeeding can help with long term weight loss but not in every case, especially when total sleep averages under 6 hours and snacking fills the gaps left by chaotic schedules.
Perimenopause and menopause introduce another set of rules. Estrogen decline shifts fat storage from hips and thighs to the abdomen, with more visceral fat around the organs. Even if you have not changed diet or exercise, you may notice a soft ring at the waist and higher fasting glucose. That is not moral failure, it is metabolic drift. It responds to targeted training, protein optimization, and in some cases medical weight loss treatment that improves insulin and appetite signaling.
The metabolism behind the mirror
Calories still matter, but focusing only on calories misses the levers that change appetite, movement, and adherence. Protein affects satiety hormones and helps maintain lean mass. Resistance training teaches your body what you want to keep when you lose weight. Sleep modulates ghrelin and leptin within days, which is why four nights of five hour sleep can spike hunger even if you are determined.
Resting metabolic rate in women ranges widely, often 1,200 to 1,700 calories per day depending on height, age, and lean mass. Two women of similar weight can differ by 200 to 300 calories in daily burn. That is the difference between progress and plateau. A supervised weight loss program accounts for this with a measured or well estimated basal rate, then sets a deficit modestly below it. The goal is sustainable weight loss, not white knuckle dieting.
Insulin and glucose control matter not because carbs are evil but because large, frequent glucose spikes can increase hunger, cravings, and fat storage over time. In practice, this means structuring meals to include protein, fiber, and healthy fats, then placing starches where you use them best, such as around activity or earlier in the day if sleep is fragile.
What counts as safe weight loss
Many women arrive having tried rapid weight loss challenges that promised 10 pounds in 10 days. The short term scale drop mostly reflects water and glycogen, not fat. Safe weight loss usually averages 0.5 to 1 percent of body weight per week. A 190 pound woman may see Grayslake weight loss experts 1 to 2 pounds weekly in the early phase, then 0.5 to 1 pound as she gets lighter. There will be weeks with little visible change, especially during the luteal phase or high stress periods. Measuring waist, hip, and thigh circumferences, noting how clothing fits, and tracking strength improvements gives a truer picture than the scale alone.
A clinical weight loss plan pays attention to lab safety as well: iron status, thyroid function, A1C or fasting glucose, lipid panel, liver enzymes, vitamin D, and in some cases cortisol patterns or reproductive hormones if cycles are irregular. Correcting a B12 deficiency or iron deficiency anemia can fix fatigue that would otherwise sabotage movement and recovery.
Building a custom weight loss plan that adapts to hormones
A personalized weight loss approach does not mean inventing a brand new diet. It means setting the right targets and matching them to your life stage and weekly rhythms.
Start with protein. Aim for 1.2 to 1.6 grams per kilogram of goal body weight per day for most women, slightly higher if you are in perimenopause or doing resistance training. For a 160 pound target, that is roughly 90 to 115 grams daily. Distribute it across three meals and one optional snack to steady appetite. Build each plate around 25 to 35 grams: eggs and Greek yogurt at breakfast, a salad with salmon or tofu at lunch, chicken thighs, lentils, or tempeh at dinner. Women often under eat protein, then feel intense cravings late afternoon and evening.
Next, choose a carbohydrate strategy that supports energy without rollercoasters. For most, 100 to 200 grams daily works, adjusted for training volume. Within that range, favor minimally processed starches and fruit. Place a larger portion around workouts or before your most demanding part of the day. Fiber targets of 25 to 35 grams help with satiety and gut health, but do not jump from 10 to 30 overnight or your gut will protest. Increase water and pace the change across 2 to 3 weeks.
Fat fills the rest of your calories. Prioritize monounsaturated and polyunsaturated sources: olive oil, avocado, nuts, seeds, and fatty fish. Women with gallbladder issues may feel better keeping fat portions on the moderate side and spacing them across meals.
Exercise should serve your metabolism, not punish it. Two to three days of resistance training, 30 to 45 minutes, builds and protects lean mass. Focus on compound movements you can load safely: squats to a box, dumbbell rows, presses, deadlifts with a trap bar, and step ups. Add 6 to 10 thousand steps most days and one or two short conditioning sessions at a conversational pace. During the luteal phase, some women benefit from a slightly lower intensity week with more walking and mobility, especially if sleep is off or cramps are strong.
Sleep and stress management are not soft add ons. In clinic, improving sleep from 5.5 to 7 hours often nudges weight loss forward even when food looks the same. A pre bed routine that reliably shortens sleep latency by 10 minutes pays off downstream. I ask patients to pick a single anchor: a 10 minute wind down with light stretching, a warm shower, or a rule to power down screens by a set time. Reducing substances that fragment sleep, like late alcohol, matters more than most realize.
How the menstrual cycle fits into your plan
Map your cycle data to your habits. During the follicular phase, your training can carry a bit more volume, and some women handle slightly lower calories without extra hunger. During the luteal phase, hunger and cravings may rise. That is not a license to graze all day, but a cue to structure meals more carefully. Add a bit more protein and a smart carbohydrate like roasted potatoes or oats at lunch, which often blunts late night snacking. Salt and water intake can help with fluid shifts. If the scale jumps by two pounds on day 24, take the long view and rely on measurements and a rolling 14 day average.
If you use hormonal contraception, your fluctuations may be flatter. If you have irregular cycles, such as with PCOS, focus on consistent habits and consider weight loss treatment that improves insulin sensitivity. Metformin and inositol can be helpful for some, paired with resistance training and higher protein intake.
Perimenopause and menopause: recalibrating for the new normal
Around the mid to late 40s, cycles shorten or become erratic, sleep may splinter at 2 a.m., and mood swings can sneak up without warning. Body composition changes are common. The plan shifts in three areas.
First, tighten up protein and strength training. Aim for the higher end of the protein range and make two lifting sessions nonnegotiable. Muscle is your ally for long term weight loss and metabolic health. Second, manage alcohol and evening carbs to protect sleep. Hot flashes and night sweats worsen with alcohol, and poor sleep raises next day hunger. Third, discuss hormone therapy with your healthcare provider if symptoms affect daily function. For appropriately screened women close to the onset of menopause, menopausal hormone therapy can improve vasomotor symptoms, mood, and potentially make weight management easier indirectly through better sleep and activity.
Some women also benefit from medical weight loss medications during this stage, especially if they have metabolic risk factors, binge eating tendencies, or long plateaus despite excellent execution. This is where physician guided weight loss, within a clinical weight loss setting, can change the trajectory.
Medical and non surgical weight loss: who benefits and how to think about it
The food and exercise fundamentals apply to everyone. That said, modern medical weight loss is more effective and safer than the crash diets of the past. A weight loss clinic that offers doctor supervised weight loss now has tools that directly affect appetite, satiety, and glucose control.
Options include GLP‑1 receptor agonists and related agents that slow gastric emptying, improve insulin response, and reduce hunger. Average total weight loss in trials ranges around 10 to 20 percent of starting weight over 12 to 18 months, with individual variability. For some women with obesity, these medications unlock behaviors they already know how to do by turning down constant food noise. Others may respond better to naltrexone bupropion or phentermine topiramate under supervision. Metformin remains helpful in insulin resistance and PCOS. The right choice depends on medical history, side effect tolerance, and goals.
Non surgical weight loss also includes structured meal replacement protocols, short term low calorie regimens with close monitoring, and weight loss counseling integrated with cognitive behavioral strategies. These are not for everyone. If you have a history of disordered eating, choose a weight loss provider with expertise in eating disorders and be cautious about rigid protocols. A good weight loss practice screens for this at intake.
When starting medication, plan for the long game. The body adapts to a lower weight by nudging appetite up and calorie burn down. People who stop medication often regain some weight unless they have built resilient habits or continue a lower maintenance dose. That is not failure. It reflects biology. A weight management program that includes coaching, nutrition support, and strength training gives you the best chance of long term weight loss.
What a professional weight loss assessment includes
A thorough weight loss evaluation looks beyond the scale. Expect a clinician to review medical history, past weight loss attempts, menstrual history, pregnancies, surgeries, current medications, sleep patterns, mood, and stress. Note the red flags: weight gain after starting a new antidepressant or mood stabilizer, irregular cycles with acne and hair changes suggestive of hyperandrogenism, new snoring that hints at sleep apnea, or joint pain limiting movement.
Baseline measurements should include weight, height, waist circumference, blood pressure, and body composition if available. Labs commonly include complete blood count, comprehensive metabolic panel, lipid panel, A1C or fasting insulin and glucose, TSH with or without free T4, ferritin, B12, and vitamin D. Depending on symptoms, prolactin and androgens may be appropriate. The goal is not to chase perfect numbers, it is to identify correctable barriers that make sustainable weight loss harder than it needs to be.
Designing meals you can repeat without boredom
You do not need a chef. You need three or four simple meal formats that hit your protein target and fit into your week. For breakfast, a Greek yogurt bowl with berries, chia, and a sprinkle of nuts takes three minutes and delivers roughly 30 grams of protein. On busy mornings, a shake with 30 grams whey or a pea blend, spinach, a frozen banana half, and a spoon of peanut butter can be prepped in under five minutes. Lunch can be a chopped salad with 4 to 6 ounces of rotisserie chicken, chickpeas, and olive oil vinaigrette. Dinner might be sheet pan salmon with broccoli and small potatoes, seasoned with salt, pepper, and lemon, cooked at 425 F for 15 minutes.
For women who crave sweets late, plan for it rather than pretending it will not happen. A 200 calorie target for an evening treat, like dark chocolate or a protein rich pudding, is more realistic than swearing off dessert, then eating 600 calories of snack foods after a rough day.
Hydration is not a magic fat burner, but it cuts down on false hunger and helps with fiber. A simple rule is to drink a glass of water with each meal and one between meals. If you are prone to lightheadedness late afternoon, add a pinch of salt to water once a day, especially in hot climates or on days with heavy sweating.
Movement for real life
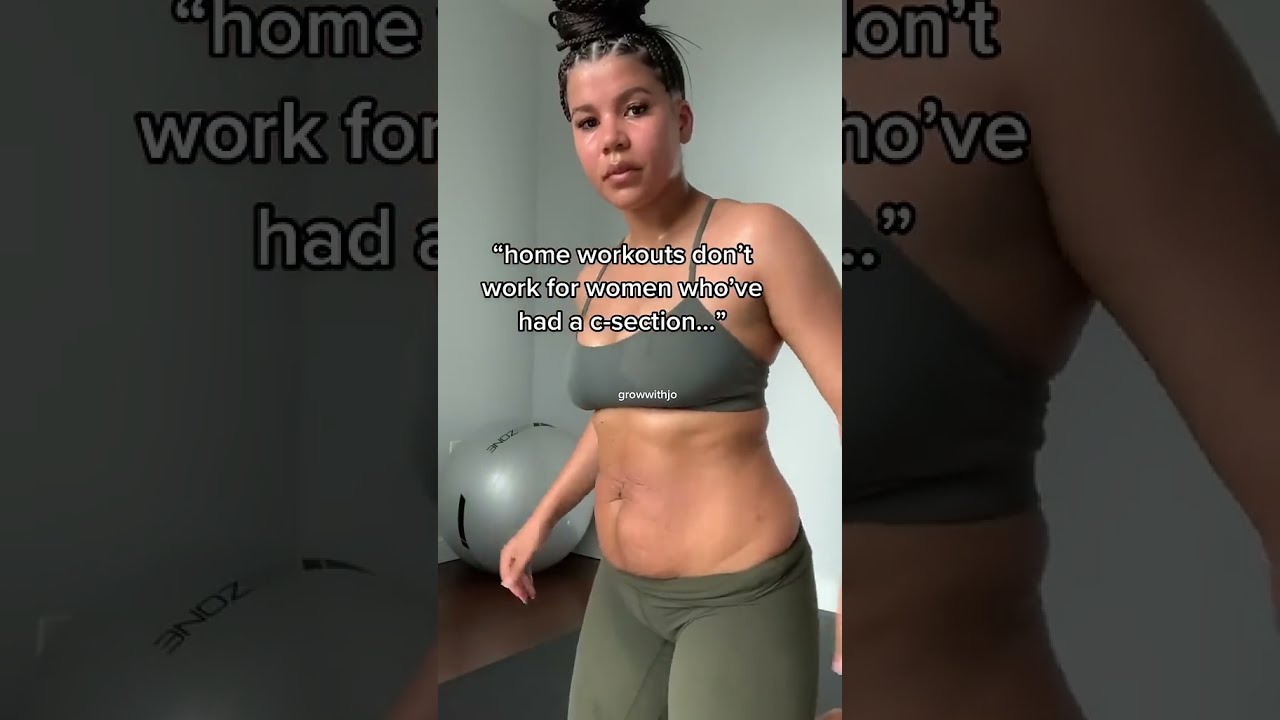
If you have not trained in years, a weight loss program that requires six days a week in a gym will not survive the school calendar. Start with steps and two brief strength sessions. Ten sets of quality work beats an hour of random fatigue. If your knees complain, we modify. Box squats to a comfortable height, incline pushups at the kitchen counter, and seated rows with a band build strength without punishment. For women with pelvic floor concerns postpartum, coordinate with a pelvic health physical therapist and begin with breath work and deep core engagement before heavy lifts.
On travel weeks, your plan needs a travel version. I ask patients to bring a short resistance band, target a minimum step count, and repeat a 20 minute hotel circuit: goblet squats with a suitcase, banded rows secured around a doorframe, incline pushups, and split squats holding the sink for balance. It is not glamorous, but it protects momentum.
When the scale stalls
Plateaus happen to everyone. The fix is not always to cut calories. Review the last 10 to 14 days. Has protein drifted down? Are weekends turning two days into maintenance or surplus? Is sleep in tatters? Somedays the answer is to add movement rather than cut food. An extra 2 to 3 thousand steps per day can bridge a small energy gap without adding hunger. If you have lost 20 or more pounds, your caloric needs are lower than when you started. A small, 100 to 150 calorie adjustment may be enough. In perimenopause, water shifts can hide fat loss for weeks. Track waist circumference and stick with the process.
Coaching, counseling, and the role of support
Data helps, but change lives in relationships. Many women benefit from weight loss coaching or structured weight loss support. A coach can see patterns you miss, like the way a skipped lunch leads to late night overeating or how work travel breaks routines. Behavioral weight loss therapy, even a handful of sessions, can shift the conversation in your head from all or nothing rules to strategic choices. If binge eating or purging behaviors appear, prioritize specialized care before any weight loss protocol.
Family and friends matter too. If your household eats dinner together, involve them in the plan rather than cooking two menus. Choose meals everyone enjoys, then adjust portions to meet your needs. If your workplace culture revolves around pastries and takeout, keep an emergency meal in your desk and decide in advance which days you will say yes.
Choosing a weight loss clinic or provider
Not every weight loss center is the same. You want a practice that offers physician guided weight loss with a thorough intake, clear explanations, and ongoing follow up. Ask how they tailor a custom weight loss plan. Do they address hormones and life stage? Can they coordinate with your primary care provider or OB‑GYN? If they prescribe medication, do they pair it with nutrition support and strength training? A clinic that measures more than weight, like waist circumference and strength metrics, tends to care about outcomes that translate into better health.
Transparent policies around side effects, cost, and follow up frequency are nonnegotiable. Beware of one size fits all protocols that ignore your history. Good weight loss services feel collaborative. You should leave a weight loss consultation with a clear plan, specific numbers, and a way to get help if something is not working.
A practical two week reset to build momentum
Use this when you need traction. It is not a cleanse or extreme dieting, it is a focused block that clarifies habits.
Set protein at 1.4 g per kilogram of goal weight and hit it daily. Anchor each meal with 25 to 35 grams of protein. Walk 8,000 steps daily, lift twice per week, and add one 20 minute cardio session at a pace that lets you talk in full sentences. Choose a consistent breakfast and lunch to reduce decisions. Rotate dinners from three quick recipes. Sleep target of 7 hours, with a 15 minute wind down on a timer. No alcohol on nights before early mornings. Track waist circumference and average weight across 7 days rather than chasing single day readings.
Two weeks is long enough to see appetite settle and energy rise. If your cycle lands mid reset, keep the structure and adjust carbs slightly upward if hunger spikes. At day 14, review. If it worked, keep going. If not, adjust protein, steps, or calories by small increments. If hunger is high and energy low, increase calories by 100 to 200 and reassess.
Results that last look boring from the outside
Successful long term weight loss rarely hinges on a secret food or supplement. It looks like stringing together dozens of small, unremarkable choices. It is bringing lunch most workdays, lifting twice a week even when it is not perfect, and refusing to catastrophize a weekend off plan. It is recognizing that hormones matter and working with them. It is getting help when personal tools are not enough, whether that is a supervised weight loss medication, a nutritionist’s eye on your portions, or counseling that untangles stress eating.
One of my patients, a 48 year old project manager, lost 42 pounds across 14 months while navigating perimenopause, a parent’s illness, and a demanding job. There were months when the scale barely moved. She kept training, upped her protein to 115 grams, and used a low dose medication for six months to dampen late day cravings. She maintained most of her loss a year later because she owned the habits, not the novelty.
You deserve a plan that respects biology, fits your life, and produces results that stick. If you want guidance, seek a professional weight loss provider who will listen, measure what matters, and stand with you for the long haul. Evidence based weight loss is not flashy. It is effective, humane, and entirely possible for women at every stage.